A school nurse once told a story about a child who came in for a scraped knee and left her office with a snack, a sticker, and a “See you tomorrow.” What stuck with the nurse was not the knee. It was how the child kept glancing at the door, like they were bracing for someone to appear. When asked a simple question, the child answered quickly, then looked down as if they had said too much.
That is what makes recognizing abuse so hard. It rarely arrives with a clear announcement. It shows up through small signals, scattered across days, sometimes weeks. Adults who spend time with children often notice the change before they can explain it: a child who becomes quieter, a teen who suddenly stops trying, a kid who flinches at normal movement. These early observations are a core focus of the National Child Abuse Mandated Reporter Training (MRT). This article focuses on the physical and behavioral signs that can point to harm, how those signs can differ by age, and how to respond in a way that protects children while staying calm, professional, and grounded in observable facts.
Understanding What Signs Really Mean
It helps to start with a simple truth: a “sign” is not the same as proof. A child can have bruises from soccer, anxiety from a move, and mood swings from hormones. At the same time, those same things can also be signals of something far more serious. The difference often lives in pattern, context, and persistence.
When adults rush to certainty, they often swing too far in either direction. Some dismiss concerns too quickly because they do not want to imagine harm. Others panic and treat a single clue as a verdict. A steadier approach is to notice what repeats, what escalates, and what does not fit the child’s developmental stage or normal baseline.
Signs Of Child Abuse That Show Up In Daily Life
The signs of child abuse often appear in ordinary settings, not dramatic ones. They show up at drop-off, in the hallway at school, in a clinic waiting room, on the sidelines of a game, or during a routine conversation that suddenly feels tense. In many cases, the child is still laughing sometimes, still participating sometimes, still doing “normal kid” things, which can make the risk feel easy to ignore.
What tends to stand out is the mismatch. A story that changes slightly each time. A child who seems careful in a way that does not match their age. A teen who shrugs off everything but looks exhausted behind the shrug. When you see several small mismatches stacking up, it is worth pausing and treating them as meaningful information.
Physical Signs That Merit A Closer Look
Children get bumps and bruises. That is part of growing up. What raises concern is where injuries occur, how often they appear, and whether the explanation makes sense for the child’s age and abilities. A bruise on a shin after recess is common. A bruise on an ear or neck is less common. A pattern of injuries in different stages of healing carries more weight than a single injury.
Physical signs can also be tied to timing and context. Some children show up with injuries after weekends, holidays, or breaks. Some have delayed care for serious injuries. Some seem unusually fearful when a caregiver is asked a basic question. None of these details confirm abuse on their own, yet they can help you notice risk with greater accuracy.
Physical indicators that often raise concern include:
- Bruises on the ears, neck, torso, back, inner arms, inner thighs, or genital area
- Marks with recognizable shapes, such as handprints, linear marks, loop marks, or clustered bruises
- Burns with defined edges, repeated patterns, or immersion-like lines on hands, feet, or buttocks
- Frequent injuries that appear without a clear pattern of play or activity
- Injuries that do not match the child’s developmental stage, such as bruising in non-mobile infants
Behavioral Changes That Often Speak First
Behavior is often the earliest place distress shows up. Some children become quiet and overly compliant, like they are trying to avoid being noticed. Others become reactive, impulsive, or angry, like their nervous system is constantly bracing for the next blow, whether physical or emotional. Both responses can be survival strategies.
A key clue is change. A child who has always been shy is different from a child who suddenly stops talking. A teen who has always been moody is different from a teen who becomes unreachable, detached, or suddenly reckless. When a shift is abrupt, persistent, or paired with other concerns, it deserves attention.
Behavioral and emotional signs may include:
- Withdrawal from friends, activities, or classroom participation
- Fear tied to specific people, places, or times of day
- Regression such as bedwetting, thumb sucking, clinginess, or baby talk returning
- Hypervigilance, flinching, exaggerated startle responses, or scanning adult moods
- Frequent somatic complaints like headaches or stomachaches with no clear medical cause
- Age-inappropriate sexual behavior or knowledge
- Self-harm statements, substance use, or risky behavior in adolescents
How Neglect Can Look Different From Other Harm
Neglect can be harder to spot because it can look like “messy life” instead of intentional harm. Yet neglect can be deeply damaging, especially when it is ongoing. It may show up as chronic hunger, poor hygiene, inappropriate clothing for the weather, untreated medical issues, or frequent absences without clear reasons.
Neglect also affects how a child functions day to day. You may see constant fatigue, difficulty concentrating, irritability, or social withdrawal. Some children become unusually independent, not because they are mature, but because they have learned they cannot rely on adults to meet basic needs.
Signs By Age And Developmental Stage
The same experience can look very different depending on a child’s age. Young children often show distress through sleep, appetite, toileting changes, clinginess, or fear around routine caregiving tasks. They may become suddenly frightened of bathing, dressing, or being picked up. They may also express distress through play themes that repeat, even when they cannot explain the theme.
School-age children may show a drop in grades, more frequent conflicts with peers, or strong fear of making mistakes. They may become perfectionistic or unusually worried about “getting in trouble.” Teens may isolate, become irritable, or take risks that seem out of character. For teens, emotional numbness can be just as concerning as anger. A teen who stops caring about anything may be carrying more than they can name.
Patterns That Matter More Than A Single Incident
Single incidents can mislead. Patterns tend to clarify. When concerns repeat across time, settings, or observers, the likelihood that something serious is happening rises. A child who comes in with an injury once may have had an accident. A child who repeatedly has injuries with vague explanations, paired with fearfulness or withdrawal, deserves careful attention.
Two practical ways to focus on patterns without guessing motives are to track frequency and to compare explanations to developmental reality. This keeps your thinking anchored in observable facts rather than assumptions. It also supports clearer documentation and stronger reporting when needed.
How To Talk With A Child Without Turning It Into An Interview
Many adults feel the urge to ask lots of questions when a child hints at harm. That urge is understandable, yet heavy questioning can overwhelm a child or lead them to change details in an effort to please the adult. Children often test safety before they disclose. They may share a small piece, watch your reaction, then decide whether to continue.
A steadier approach is to listen, reflect, and keep questions minimal. You can say, “Tell me more about that,” or “What happened next?” if you need a basic safety detail, but avoid leading questions or “why” questions. If a child shares something concerning, calm phrases can help: “I’m glad you told me,” “You did not do anything wrong,” and “I can’t keep this secret, but I can help.”
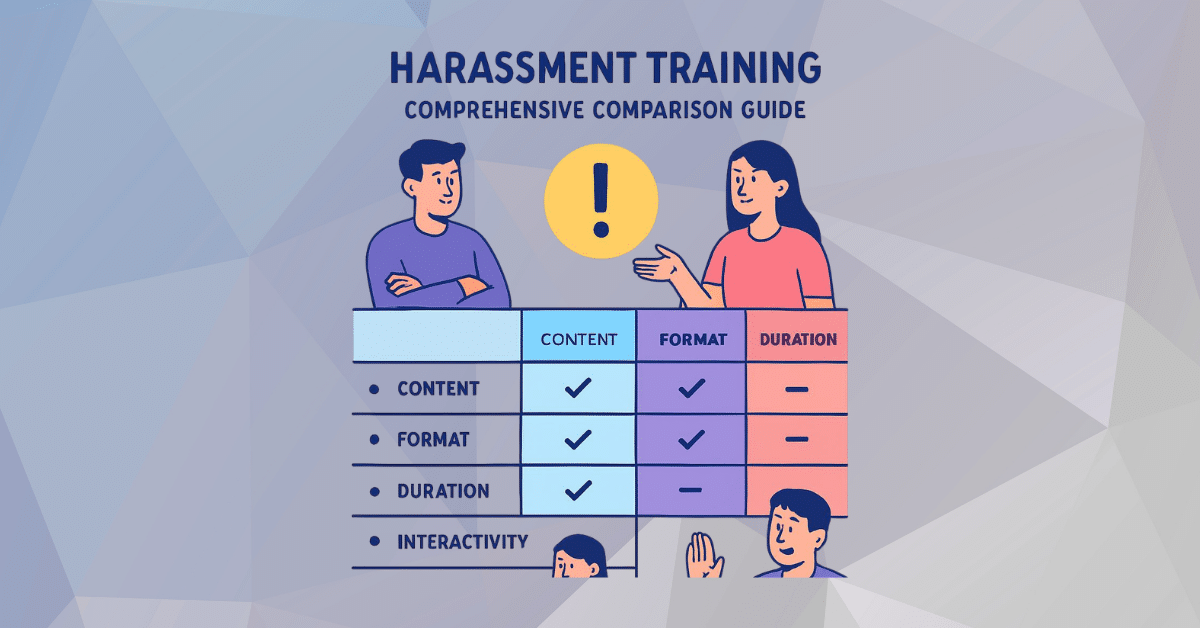
Documenting Observations Clearly And Calmly
Strong documentation is plain and specific. It avoids interpretation and sticks to what you saw and heard. Write direct quotes when possible. Describe injuries by location, size, color, and shape. Note the child’s affect and behavior in simple terms: trembling, guarded posture, tearful, unusually flat tone, or startled reaction to touch.
Many workplaces already emphasize careful records in other sensitive areas, including harassment training recordkeeping, because clear notes reduce confusion and protect everyone involved. The same discipline applies here. Objective documentation supports better decision-making and helps avoid misunderstandings that can harm a child or derail a response.
Legal Responsibilities And Reporting
Mandated reporters are typically not required to prove abuse. Many systems rely on a reasonable suspicion standard, which exists so children are not left waiting for certainty while harm continues. That is where child abuse reporting laws shape real-world action. They define who must report, what is reportable, how quickly a report must be made, and what protections exist for good-faith reporting.
If you work in a setting with children, knowing your local requirements and your internal protocol ahead of time can reduce hesitation when you are under pressure. In the moment, clarity helps. It turns a frightening decision into a process with steps: observe, document, report through the correct channel, and avoid repeated questioning of the child.
Training That Helps People Respond Consistently
People often freeze because they worry about making the wrong call. Training helps when it prepares staff for gray areas, not just obvious scenarios. Case examples, documentation practice, and role-play of brief, calm responses can make a difference when a real moment arrives.National Child Abuse Mandated Reporter Training MRT
Some organizations use National Child Abuse Mandated Reporter Training MRT to reinforce consistent steps across staff and reduce the “pass the concern to someone else” problem. Consistency matters because children often interact with multiple adults, and shared expectations reduce the chance that warning signs get minimized or lost.
Practical Steps When You Suspect A Child Is Not Safe
When you suspect harm, it helps to focus on what you can control: safety, observation, and procedure. If a child is in immediate danger, emergency steps come first. If danger is not immediate, the next step is timely reporting through your organization’s process.
A practical approach often includes:
- Staying calm and keeping your tone neutral
- Listening without pressing for details
- Documenting what you observed and what was said using direct quotes
- Reporting promptly through the correct channel
- Limiting how many adults ask the child questions, to reduce stress and confusion
Prevention And Protective Factors
Prevention is not only a public awareness campaign. It lives in daily environments where children feel seen and supported. Predictable routines, stable relationships, and access to resources can lower risk. Children are also more likely to speak up when they believe adults will respond without panic or punishment.
Protective factors can include safe adult connections at school or in community settings, caregiver support services, and age-appropriate education about boundaries. When children have trusted adults and clear pathways to help, secrecy becomes less powerful.
Conclusion
Recognizing physical and behavioral signs of abuse is rarely about a single dramatic clue. It is about noticing patterns, staying grounded in observable facts, and responding through the appropriate process when concerns arise. Children often communicate distress in fragments, and adults who pay attention to those fragments can change outcomes.
If you work with children, keep your steps simple: watch for changes, document clearly, and follow reporting procedures when reasonable concern exists. A child does not need a perfect adult. A child needs an adult who notices, stays steady, and takes action when safety may be at risk.
FAQ
What Are The Most Common Signs Of Child Abuse Adults Notice First?
The most common signs of child abuse are often changes in a child’s baseline rather than a single dramatic event. Adults may notice a child becoming unusually withdrawn, fearful, or jumpy, or a teen becoming detached and emotionally flat. Repeated injuries can also stand out, especially when explanations feel vague or inconsistent. A single sign is not proof, but patterns that repeat or cluster over time deserve documentation and a report through the proper channel when reasonable concern exists.
Can Behavioral Changes Be Signs Of Child Abuse Even Without Visible Injuries?
Yes, behavioral changes can be some of the earliest signs of child abuse, even when there are no visible marks. Children may regress, become unusually anxious, or seem constantly on edge. Some become overly compliant, while others become angry or impulsive. Teens may withdraw, stop engaging in school, or take risks that feel out of character. When a behavioral shift is sudden, persistent, or paired with other concerns, it can signal that the child is coping with something unsafe.
How Can Adults Tell The Difference Between Normal Bruises And Signs Of Child Abuse?
Normal bruises often show up on bony areas like shins, knees, and elbows, especially in active children. Signs of child abuse can include bruises in less typical areas like the ears, neck, torso, back, or inner thighs, or marks with clear shapes such as handprints or linear patterns. Frequency matters too. Injuries appearing repeatedly, especially with changing explanations or different stages of healing, should be documented carefully and handled through reporting procedures.
What Should Someone Do If They Notice Possible Signs Of Child Abuse?
If someone notices possible signs of child abuse, the most helpful next step is to stay calm and focus on facts. Document what you observed, including dates, details, and direct quotes if the child disclosed something. Avoid pressing the child for more details or asking leading questions. Follow your organization’s protocol and mandated reporting steps if applicable. Reporting is not about proving abuse. It is about sharing concerns so trained professionals can evaluate safety and respond appropriately.
Do Signs Of Child Abuse Look Different In Teens Than In Younger Children?
They often do. Teens may show signs of child abuse through withdrawal, sudden anger, risky behavior, substance use, or statements about self-harm. Some become emotionally numb or stop caring about activities they once valued. Younger children may show fear, regression, clinginess, sleep disruption, or intense reactions to routine care. In any age group, the most meaningful clue is change from the child’s normal baseline, especially when multiple signs appear together and persist.